Orthopedic Oncology: Reducing Lead Times to Deliver Personalized Solutions
In the world of orthopedic oncology, patient-specific solutions are changing the game. Personalized approaches help surgeons navigate complex surgeries and improve patient outcomes. However, one major roadblock in scaling patient-specific solutions is the long lead times to deliver personalized solutions for surgery.
Delays in preoperative planning can add stress and uncertainty to an already challenging situation. So, what’s the secret to speeding things up without sacrificing quality?
The answer lies in the intelligent use of AI and cutting-edge three-dimensional preoperative planning technology.
Why patient-specific matter in orthopedic oncology
Before diving into how we can reduce lead times, it’s essential to understand why patient-specific solutions are so critical in orthopedic oncology, particularly in complex cases.
Orthopedic oncology deals with the treatment of bone tumors, which can often require surgeons to perform intricate procedures. In these cases, a one-size-fits-all approach does not always work. Every patient’s anatomy and tumor characteristics are unique. This is where patient-specific solutions come into play.
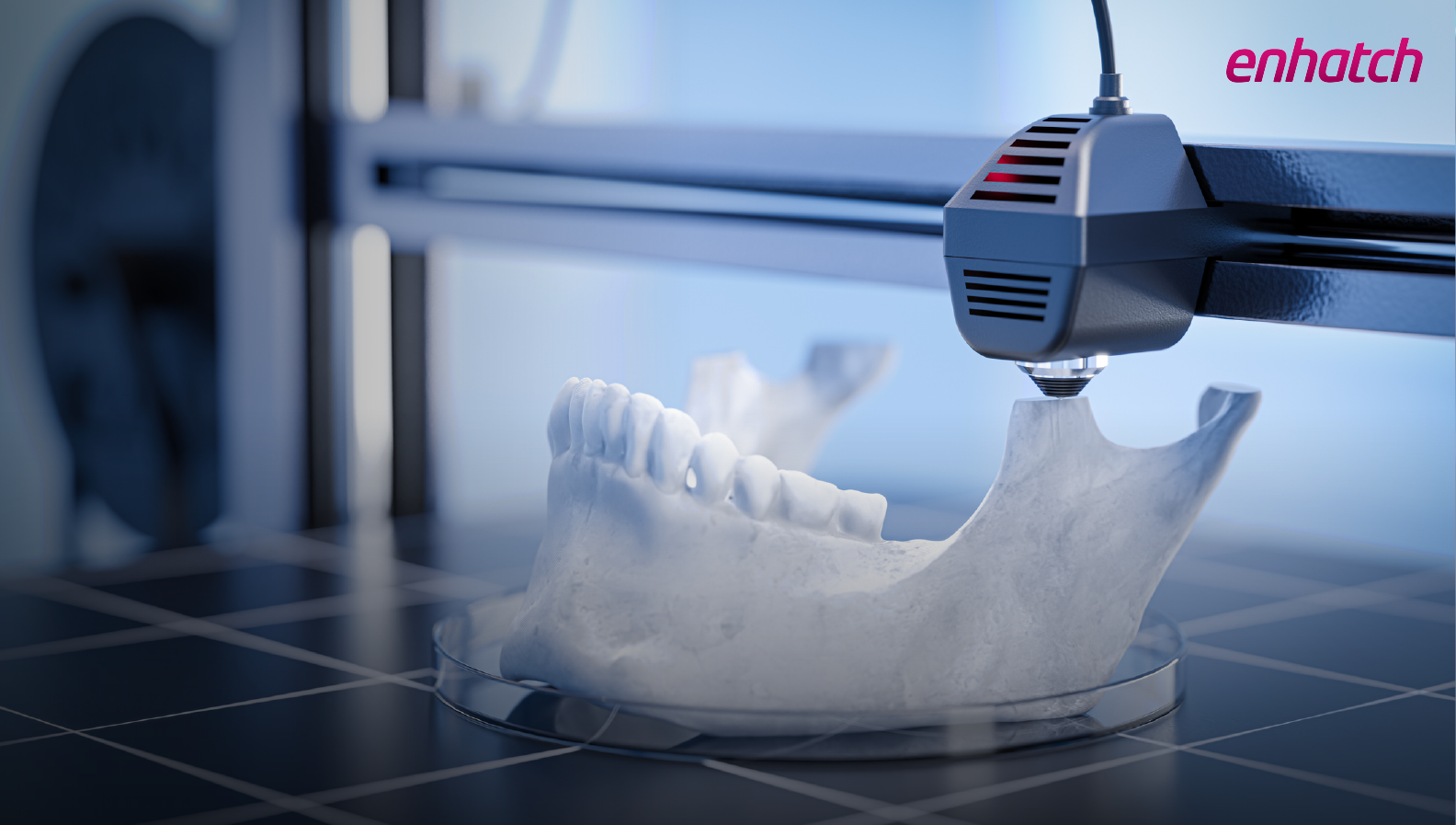
With advances in 3D printing and preoperative planning technology, surgeons can tailor treatment plans to match a patient’s anatomy.
For example, 3D anatomical models help surgeons with better surgical preparation as they can better understand the patient’s unique anatomy. Patient-specific guides can help reduce operation time and bone loss during surgery.
However, despite of all these benefits, scaling patient-specific solutions in orthopedic oncology has been a challenge due to the long lead times involved.
The lead time challenge
One of the most significant challenges in delivering patient-specific solutions in orthopedic oncology is the lengthy lead time required for preoperative planning, design, and production of 3D-printed implants. These are some of the reasons that can explain the length of the process:
- The creation of 3D anatomical models: High-quality CT or MRI scans create 3D anatomical models of the patient's bone structure and tumor. Traditionally, generating these models has been a manual and time-consuming process. The manual process involved skilled personnel or engineers interpreting patient scans, evaluating vital anatomic landmarks, and developing 3D models.
- Uploading patient medical scans: This is a critical first step before 3D modeling can even begin. However, incomplete or incorrect information can occur during the upload process. Teams from the medical device company must verify the files, and if any discrepancies are found, they have to ask surgical teams to resubmit accurate data. This back-and-forth can cause unnecessary delays.
- Collaboration between multiple stakeholders: In a typical patient-specific surgery, the surgeon collaborates with various stakeholders (radiologists, engineers, and implant manufacturers) to ensure everything is ready for the surgery. This collaboration can sometimes be a challenge and increase the lead time of the process.
This process can take several weeks. Reducing the lead time for preoperative planning is essential for scaling patient-specific surgeries in orthopedic oncology.
Time is of the essence
Time is a critical factor in orthopedic oncology, especially during procedures like limb salvage surgery. When dealing with tumors, every moment counts. Delaying treatment can lead to tumor progression, which might limit options down the line.
In limb salvage surgery, the goal is to remove the cancer while preserving as much function as possible. The longer we wait, the more complicated the surgery can become. Already, limb salvage procedures can have a significant failure rate. Research has shown that these rates can range from 24% to 42%, influenced by factors such as the technique used and the anatomical site of the tumor.
Similarly, head and neck squamous cell carcinoma (HNSCC) accounts for almost 3% of new cancer diagnoses in the United States. Studies have shown a 29% increase in mortality for certain tumor locations when oropharyngeal surgery was delayed by more than 30 days. This increase was relative to surgery performed within 30 days. Also, the study predicted that patients with a time to surgery longer than 67 days could experience worse overall survival than those with a time to surgery of 67 days or less.
There's the emotional aspect to consider. Patients are often anxious and eager to move forward. The sooner we can act, the sooner they can begin the healing process. Timely intervention in orthopedic oncology is about improving outcomes and preserving patient quality of life.
Leveraging technology to reduce lead time
Integrating Artificial Intelligence (AI) in preoperative planning
Artificial intelligence is a powerful tool that has the potential to dramatically reduce lead times in patient-specific surgeries. The primary advantage is its ability to process vast amounts of data quickly and efficiently, making it a perfect fit for the complex workflow of patient-specific solutions.
Take, for instance, the creation of 3D anatomical models. AI can speed this up significantly. With AI-powered algorithms, 3D models can be generated almost instantly, helping surgeons and engineers visualize the patient's anatomy.
Imagine a scenario where a patient's CT scan is uploaded, and potentially, within minutes, an AI tool generates a detailed 3D model of the patient's tumor and surrounding bone structure. Such rapid modeling enables quicker decision-making, reducing the time from diagnosis to treatment planning.

Image: Preoperative planning session using a knee 3D model generated by Enhatch's AI-powered segmentation tool.
An intelligent 3D planning solution with a DICOM viewer can also verify patient data immediately after uploading it. Rapid identification of data issues saves valuable time and prevents unnecessary back and forth.
At Enhatch, we have integrated AI into our preoperative planning solution. As a team, we see immense potential in leveraging AI to reduce lead times in orthopedic oncology. Our AI-powered 3D planning solution can generate 3D anatomical models quickly, not only from CT scans and MRIs but also from X-rays. United Orthopedic Corporation has recently leveraged Enhatch's technology to launch patient-specific guides for knee surgery.
Enhancing collaboration with streamlined 3D planning
AI isn’t the only technological advancement poised to change how we approach patient-specific surgeries. Cutting-edge preoperative planning solutions play an equally critical role in improving communication and collaboration among all the players involved in the surgery.
Historically, facilitating collaboration between all key stakeholders for patient-specific orthopedic oncology surgeries has been challenging. But new preoperative planning software is changing that by offering a centralized platform where everyone can collaborate seamlessly.
These platforms allow surgeons to review patient scans, 3D models, and discuss surgical strategies with their team—all in one place. Everyone from the engineers designing the cutting guides or implants to the radiologists can be on the same page, reducing the chances of miscommunication or delays. With intuitive dashboards, cases, roles, approvals, and progress can all be easily tracked.
The result? A smoother, more streamlined planning process that reduces lead times and improves overall efficiency.
Recently, Clarkson College used Enhatch's 3D planning solution to collaborate and create patient-specific cutting guides for a complex pediatric oncology surgery.
This complex case involved surgery on a 10-year-old pediatric patient diagnosed with osteosarcoma from a proximal tibial bone lesion. The tumor was in proximity to the physis and proximal tibial joint. As accuracy in resection and reconstruction of the diseased tibial bone was crucial, a patient-specific approach was preferred by the Clarkson College team.
Enhatch's preoperative planning portal streamlined the planning process of this complex oncology and contributed to the success of the surgery.
A faster path to surgery
So, what does all of this mean? This means that patients can get the life-saving surgeries they need faster. By leveraging AI to accelerate 3D model generation and utilizing advanced preoperative planning solutions to enhance collaboration, we can significantly reduce the time it takes to move from diagnosis to surgery. This is especially important in orthopedic oncology, where tumors can progress rapidly, and timely intervention can make all the difference.
Surgeons can perform these complex, life-altering procedures more efficiently and accurately. When surgeons can access accurate 3D models and work seamlessly with their team, they’re better equipped to execute the surgery with precision, leading to improved patient outcomes.
As AI and advanced preoperative planning solutions evolve, we can expect even greater efficiency and shorter lead times to deliver patient-specific solutions for orthopedic oncology surgeries.
Sources
-
“Time is crucial in malignant tumor cases: Speeding up the process of patient-specific implant creation” retrieved from the NIH website. Visit Page
-
“Reconstructive Science in Orthopedic Oncology” retrieved from the NIH website. Visit Page
-
“3D-printed guiding templates for improved osteosarcoma resection,” retrieved from the NIH website. Visit Page
-
“Current Concepts in the Resection of Bone Tumors Using a Patient-Specific Three-Dimensional Printed Cutting Guide.” Visit Page
- “Patient-specific guides in orthopedic surgery” retrieved from the Sciencedirect website. Visit Page
- “Limb salvage in musculoskeletal oncology: Recent advances” retrieved from the NIH website. Visit Page